About Mandakini Medi Engg Health Pvt Ltd
- To be world leaders in salvaging limbs & reduce the rate of amputations.
Transient Ischemic Attack - Mandakini Foot Care
- Home
- Transient Ischemic Attack
- mandakinifootcare
- 0 Comments
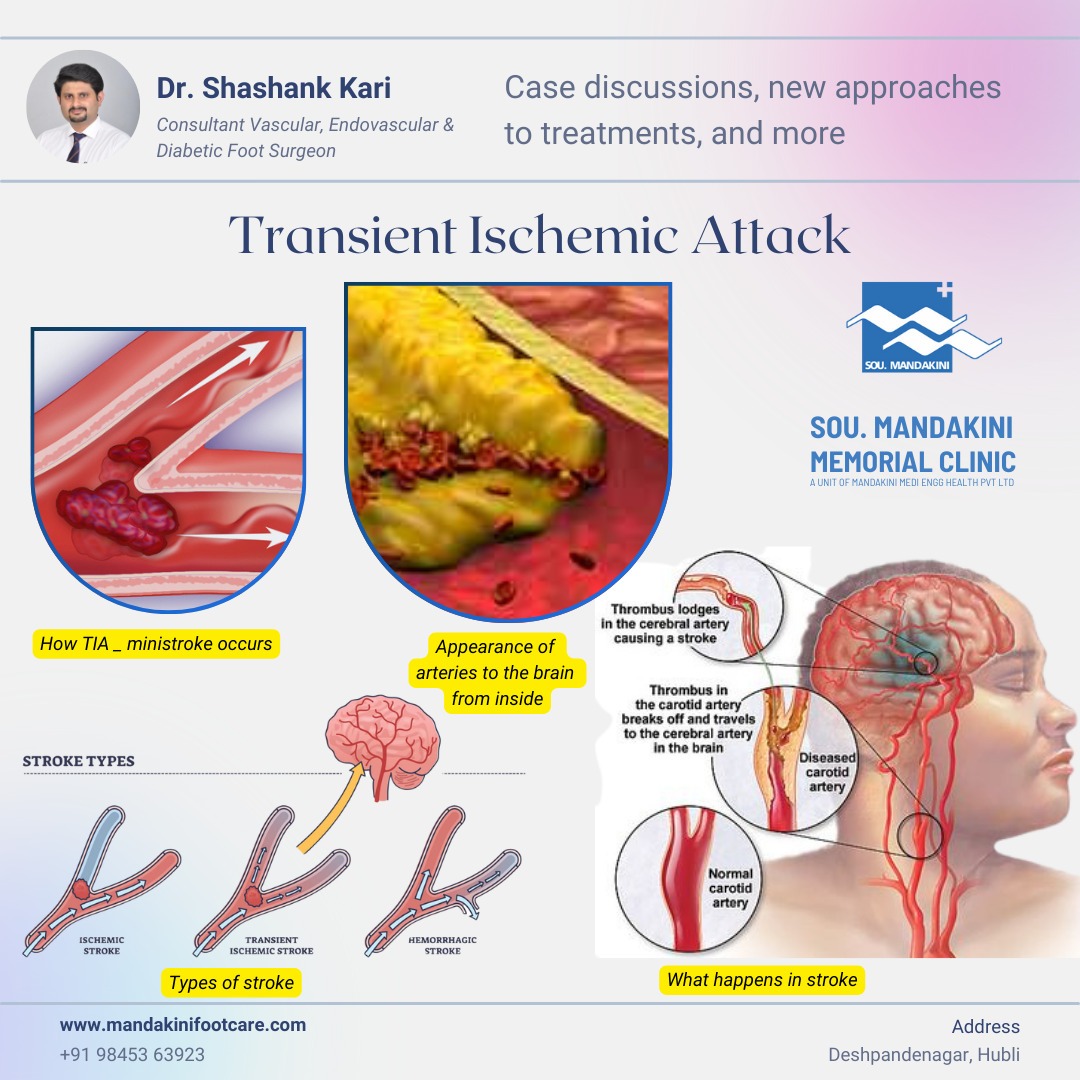
Transient Ischemic Attack
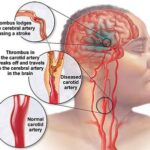
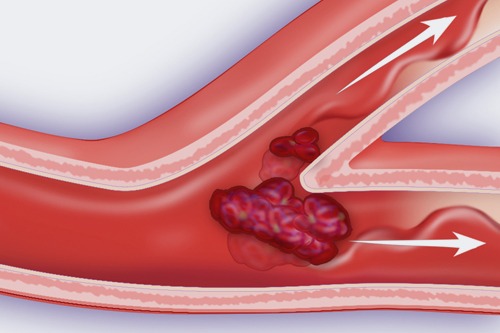
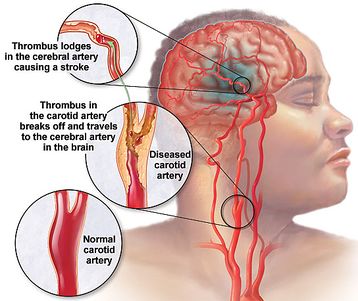
A Transient Ischemic Attack (TIA) is often referred to as a mini-stroke. It occurs when there is a temporary decrease in blood flow to a part of the brain. This temporary disruption can cause stroke-like symptoms, such as sudden weakness or numbness in the face, arm, or leg, typically on one side of the body. Other symptoms may include difficulty speaking, confusion, and sudden vision changes.
TIAs are different from strokes primarily in that they do not cause permanent brain damage. However, they are often considered warning signs of an increased risk of a full-blown stroke in the future. It's crucial to seek immediate medical attention if you or someone else experiences symptoms of a TIA, as prompt treatment can help prevent a stroke.

Risk factors for TIAs and strokes include high blood pressure, high cholesterol, diabetes, smoking, and a history of heart disease or previous strokes. Management typically involves lifestyle changes, medications to control risk factors, and sometimes surgical interventions to reduce the risk of future strokes. Regular medical follow-up and adherence to treatment plans are essential for managing TIAs effectively.
1. *Clinical Presentation*: Patients often present with sudden onset of focal neurological deficits that resolve within 24 hours. Symptoms can include transient weakness or numbness of the face, arm, or leg, usually on one side of the body. Other common symptoms include difficulty speaking or understanding speech, temporary loss of vision in one eye or both eyes, and transient dizziness or loss of balance.
2. *Risk Factors*: Discussion would involve identifying and addressing underlying risk factors such as hypertension, diabetes mellitus, hyperlipidemia, smoking, atrial fibrillation, and other cardiovascular diseases. Assessing these factors is crucial as they predispose individuals to both TIAs and full-blown strokes.
3. *Diagnostic Workup*: Evaluating the patient typically involves neuroimaging (e.g., MRI or CT scan) to rule out acute ischemic stroke and to identify any potential infarcts or other abnormalities. Additional tests may include carotid ultrasound to assess for stenosis, echocardiography to detect potential cardiac sources of emboli, and laboratory tests to evaluate for hypercoagulable states or other systemic conditions.
4. *Management and Treatment*: Immediate management focuses on preventing further episodes and reducing the risk of stroke. This often includes antiplatelet therapy (e.g., aspirin), statin therapy for cholesterol management, blood pressure control, and lifestyle modifications such as smoking cessation, dietary changes, and regular exercise. In cases where there is significant carotid artery stenosis or other specific findings, surgical interventions like carotid endarterectomy or stenting may be considered.
5. *Prognosis and Follow-Up*: Prognosis after a TIA is generally good if appropriate management is instituted promptly. However, the risk of subsequent stroke remains elevated, particularly in the early period following a TIA. Therefore, close follow-up with regular monitoring and adjustment of treatment plans is essential to minimize risk and optimize long-term outcomes.
6. *Patient Education*: Educating patients about the importance of adherence to medications, lifestyle modifications, and recognizing signs of recurrent symptoms is crucial in preventing future TIAs and strokes.
Transient Ischemic Attack new approaches to treatments
Recent advancements in the treatment of Transient Ischemic Attacks (TIAs) have focused on several key areas:
1. *Early Risk Stratification and Intensive Management*: There is increasing emphasis on rapid assessment and early initiation of treatment following a TIA. This includes risk stratification tools to identify patients at highest risk of subsequent stroke, such as the ABCD2 score (which assesses age, blood pressure, clinical features, duration of symptoms, and diabetes). Early intensive management often involves aggressive control of risk factors like hypertension, diabetes, and hyperlipidemia, which have been shown to significantly reduce the risk of stroke after a TIA.
2. *Dual Antiplatelet Therapy*: While aspirin has been a mainstay in preventing recurrent ischemic events, recent studies have explored the use of dual antiplatelet therapy (e.g., aspirin plus clopidogrel) in the acute phase following a TIA. This approach has shown promise in reducing the risk of early recurrent stroke, although the optimal duration and patient selection criteria are still under investigation.
3. *Interventional Approaches*: For patients with high-grade carotid artery stenosis identified as the cause of TIA, carotid endarterectomy or carotid artery stenting remains a standard intervention to reduce the risk of stroke. Advances in surgical techniques and perioperative management have improved outcomes in these cases.
4. *Lifestyle and Behavioral Interventions*: There is growing recognition of the importance of lifestyle modifications in reducing the risk of stroke after a TIA. This includes promoting smoking cessation, encouraging regular physical activity, promoting a heart-healthy diet, and managing stress effectively.
5. *Personalized Medicine Approaches*: Advances in genetic and biomarker research may pave the way for more personalized treatment approaches in the future, helping to tailor therapies based on individual risk profiles and underlying pathophysiological mechanisms.
These new approaches underscore the evolving landscape of TIA management, aiming not only to prevent immediate recurrent events but also to optimize long-term outcomes and quality of life for patients at risk of stroke.
Transient Ischemic Attack Prevention
Prevention strategies for Transient Ischemic Attacks (TIAs) primarily focus on reducing the risk factors that contribute to their occurrence. Here are key approaches to prevent TIAs:
1. *Control Blood Pressure*: Hypertension is a significant risk factor for TIAs and strokes. Keeping blood pressure within normal limits (usually below 140/90 mmHg, but individual targets may vary) through lifestyle modifications and medications prescribed by a healthcare provider is crucial.
2. *Manage Cholesterol Levels*: High levels of LDL (bad) cholesterol can contribute to atherosclerosis (hardening and narrowing of arteries), increasing the risk of TIAs and strokes. Lifestyle changes (such as adopting a heart-healthy diet low in saturated fats and cholesterol) and medications (such as statins) can help manage cholesterol levels.
3. *Control Diabetes*: Diabetes increases the risk of cardiovascular diseases, including TIAs and strokes. Managing blood sugar levels through diet, exercise, and medications prescribed by a healthcare provider is essential.
4. *Stop Smoking*: Smoking damages blood vessels and increases the risk of atherosclerosis. Quitting smoking can significantly reduce the risk of TIAs and strokes.
5. *Maintain a Healthy Weight*: Being overweight or obese can contribute to hypertension, high cholesterol, and diabetes, all of which increase the risk of TIAs. Maintaining a healthy weight through regular physical activity and a balanced diet can help prevent TIAs.
6. *Limit Alcohol Intake*: Excessive alcohol consumption can raise blood pressure and contribute to other cardiovascular risk factors. If you drink alcohol, do so in moderation (defined as up to one drink per day for women and up to two drinks per day for men).
7. *Exercise Regularly*: Physical activity helps maintain a healthy weight, lower blood pressure, improve cholesterol levels, and reduce the risk of diabetes. Aim for at least 150 minutes of moderate-intensity aerobic exercise (such as brisk walking) or 75 minutes of vigorous-intensity aerobic exercise (such as running) per week, as well as muscle-strengthening activities on two or more days per week.
8. *Eat a Healthy Diet*: A diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats (such as those found in olive oil, nuts, and fatty fish) can help lower cholesterol levels, reduce blood pressure, and promote overall cardiovascular health.
9. *Manage Stress*: Chronic stress may contribute to high blood pressure and other risk factors for TIAs. Practice stress-reduction techniques such as deep breathing, meditation, yoga, or spending time with loved ones.
10. *Adhere to Medical Advice*: If you have conditions such as atrial fibrillation or carotid artery disease that increase your risk of TIAs, follow your healthcare provider's recommendations for treatment and monitoring.
By adopting these preventive measures, individuals can significantly reduce their risk of experiencing TIAs and the potential for subsequent strokes, thereby promoting long-term cardiovascular health and well-being. Regular medical check-ups and discussions with healthcare providers are also crucial for assessing individual risk factors and tailoring preventive strategies accordingly.
Contact :
Dr. Shashank kari - Consultant Vascular, Endovascular & Diabetic Foot Surgeon
At : Sou. Mandakini Memorial Clinic
Deshpande nagar, Hubli, Karnataka India.
Shopping Cart
There is no item in your cart